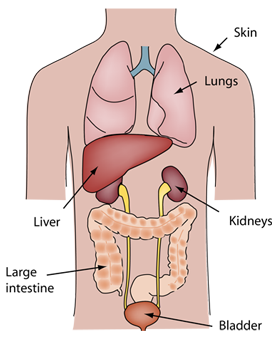
Elements of the Urinary System
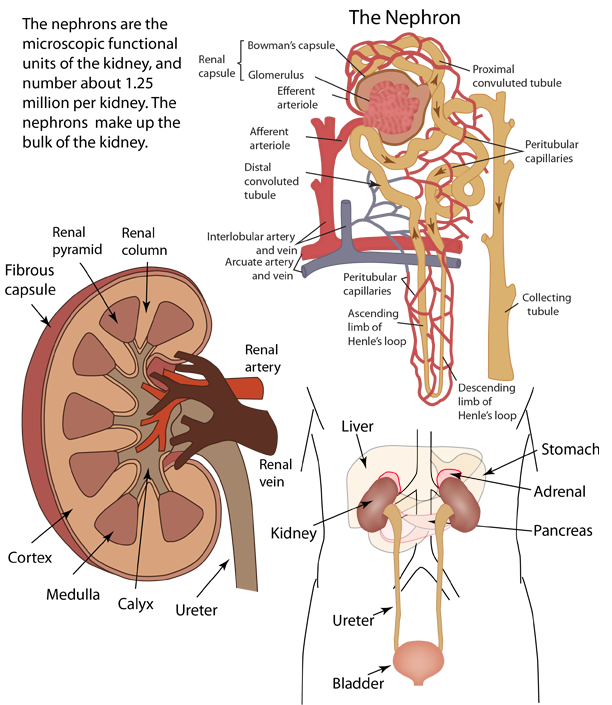
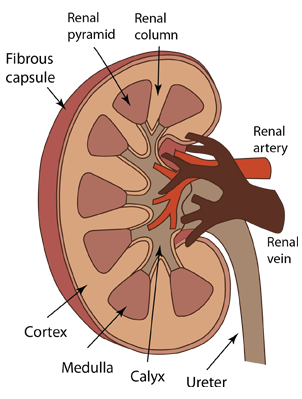
Kidney Structure
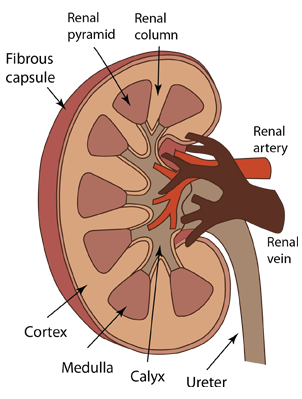 | Renal Cortex: The outer portion of the kidney which contains the beginning parts of the nephrons including the glomeruli with their enclosing Bowman's capsules. Part of the cortex extends between the structures of the medulla forming renal columns.
Medulla: Inner fan-shaped collection of structures which contain most of the later parts of the nephrons, including Henle's loop and the associated blood vessels. There are some nephrons that are contained entirely in the cortex. The individual structures of the medulla are called renal pyramids.
Calyx: cuplike structure in the inner part of the kidney where the beginning of the collection of urine for transport out of the body.
|
Renal Pelvis: The larger collection reservoir formed by the joining of the calyx units. This reservoir narrows as it exits the kidney to become the ureter.
Renal artery and Renal vein: These blood vessels are quite large and carry about 1200ml of blood per minute, or about one fifth of the total blood flow from the heart. Between the pyramids of the kidney's medulla, the renal artery branches to form interlobular arteries that extend outward toward the cortex and arch over the bases of the pyramids to form the arcuate arteries. From these arcuate arteries, interlobular arteries extend into the cortex.
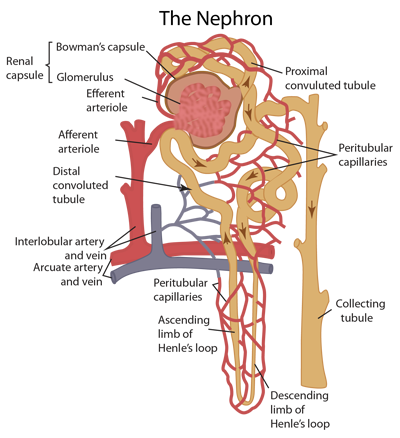
The Nephron
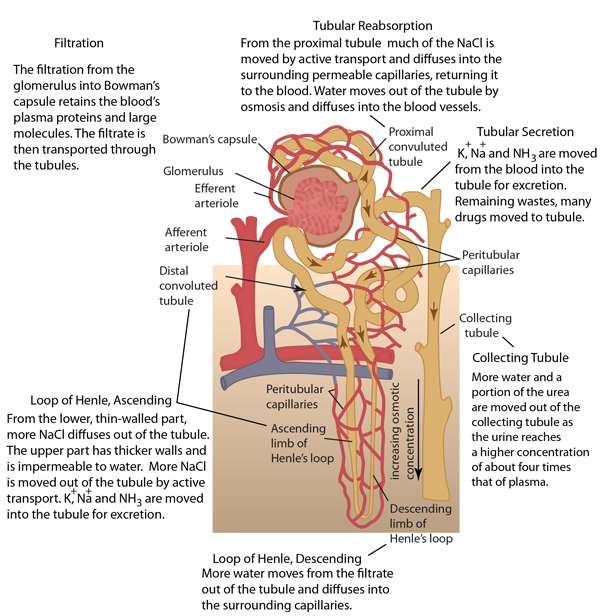
Renal capsule: The structure containing the glomerulus. The renal capsule and both proximal and distal tubules lie in the renal cortex.
Bowman's capsule: a cuplike structure which holds the glomerulus and collects the blood filtered by it.
Glomerulus: a dense knot of capillaries with a unique structure that allows them to filter the blood. The walls of the glomerular capillaries are extremely permeable to water and small dissolved molecules, but prevent the passage of large protein molecules such as the albumin in the blood.
| 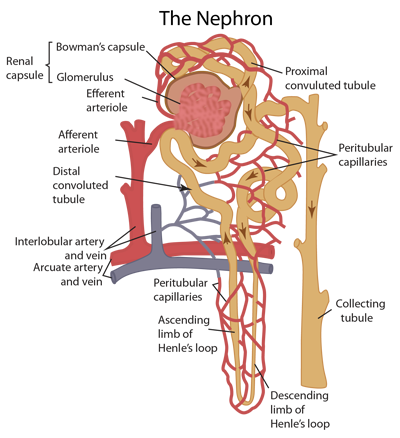 | |
Afferent arteriole: From an interlobular artery, blood enters the afferent arteriole which carries the blood into the glomerulus for filtering.
Efferent arteriole: After passing through the glomerulus, the remaining fluid with the filtrate removed is much more concentrated and passes into the smaller efferent arteriole and branches into multiple small, highly porous capillaries. These capillaries surround the tubule which has carried the filtrate from Bowman's capsule and are in intimate contact with it.
Proximal convoluted tubule: the filtrate leaving Bowman's capsule into the tubule contains nutrients and water and a portion of those are reabsorbed into the blood flowing through the nearby capillaries. This reabsorption can include salts, glucose, and amino acids which are excreted from the tubule by active transport and then diffuse into the porous capillaries. At the same time, remaining waste products including urea become more concentrated in the tubule.
Loop of Henle: just past the proximal tubule, a thinner tubule descends to a sharp turn and returns with an enlarged tubule. This structure extends into the medulla of the kidney for most nephrons. Along the loop of Henle there is more concentration of the urine by osmosis of water out of the tube and transfer of NaCl out by active transport.
Distal convoluted tubule: Beyond the loop of Henle the tubule moves to a point adjacent to the afferent arteriole and the two of them form the juxtaglomerular apparatus. This structure is important in maintaining homeostasis of blood flow because it reflexively secretes renin when the blood pressure in the afferent arteriole drops. Renin triggers a mechanism that produces angiotensin, a substance that causes vasoconstriction and a resulting increase in blood pressure.
Collecting tubule: From the distal tubule the urine enters the straight tubule that is joined by the distal tubules of several nephrons.
|